In perioperative environments, details matter—especially those that impact infection prevention and patient safety. While acrylic and artificial nails may be fashionable, in the sterile world of the OR and Sterile Processing Department (SPD), they pose a real risk.
🔬 Evidence of Patient Harm
Healthcare workers wearing long or artificial nails have been directly linked to serious infections and even fatalities in patients:
📍 NICU Outbreak (USA)
-
Pathogen: Pseudomonas aeruginosa
-
Impact: 46 infected infants; 16 deaths
-
Source: Nurses with long and artificial nails
-
Outcome: Outbreak ceased after nail-length restrictions were implemented
📍 Spinal Surgery Fungal Infections
-
Pathogen: Candida albicans
-
Impact: Multiple patients developed postoperative osteomyelitis
-
Source: OR technician with artificial nails
-
Outcome: No further cases after technician was removed
🔬 Lab-Based Evidence
Studies show that:
-
Up to 87% of healthcare workers with artificial nails harbored pathogenic organisms, even after scrubbing.
-
Natural nails showed significantly lower colonization rates.
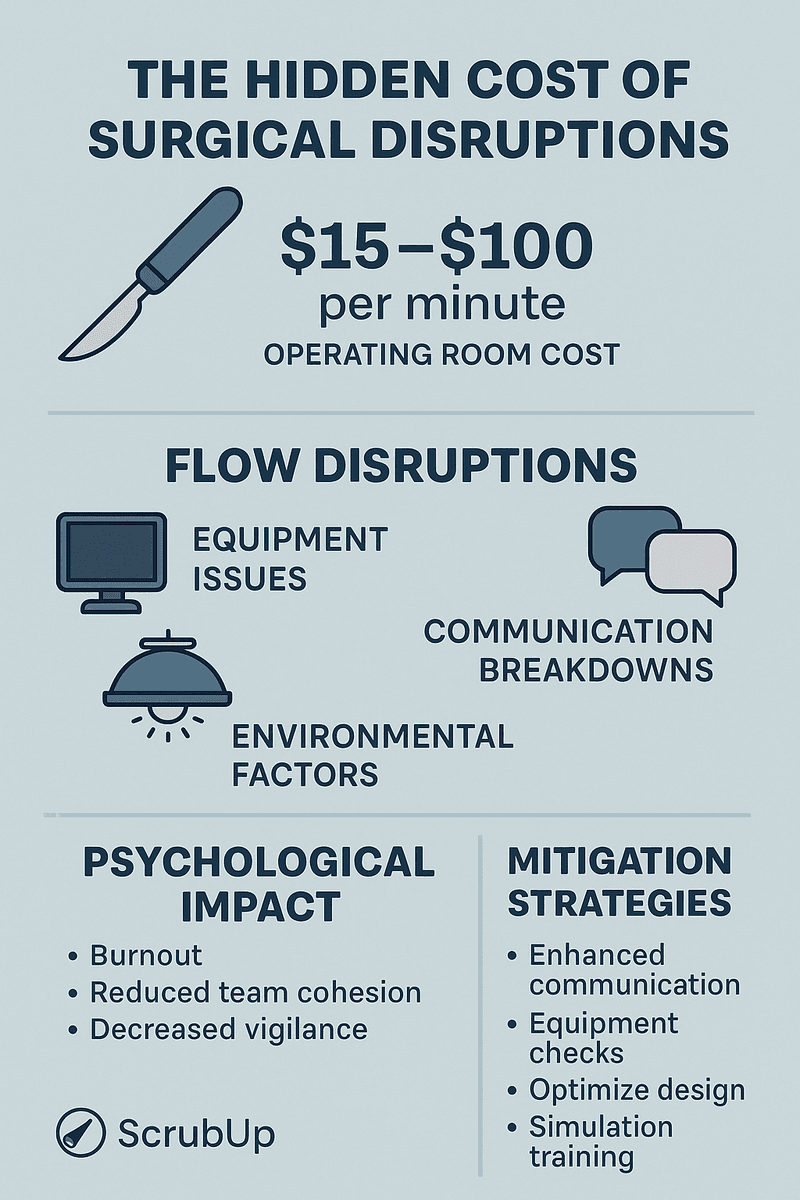
💰 The Financial Toll
Preventable infections don’t just harm patients—they’re expensive:
-
Cost per hospital-acquired infection:
AUD $18,000–$42,000+ -
10-case outbreak could cost a hospital $400,000+, not including litigation or reputational damage.
-
Surgical site infections (SSIs) cost hospitals about $20,000 per patient
-
MRSA-related SSIs can exceed $60,000 per case, with longer hospital stays and higher risk of complications
-
Even just 5–10 avoidable cases linked to policy breaches (like wearing acrylic nails) could cost a hospital hundreds of thousands of dollars
-
Infections linked to lapses in infection control—like poor nail hygiene—carry a major financial burden:
-
Hospital-acquired infections (HAIs) cost the U.S. healthcare system an estimated $28–45 billion annually 📉
📜 What the Guidelines Say
✅ AORN (USA)
“Artificial nails should not be worn by perioperative team members who have direct contact with patients.”
✅ ACORN (Australia)
“Staff in the perioperative environment must not wear artificial fingernails or nail enhancements.”
Both standards emphasize natural nails ≤ ¼ inch in length, free from polish chips or artificial coatings.
🔄 Best Practice for OR & SPD Teams
-
Keep nails natural, short, and clean
-
Avoid all artificial enhancements (acrylic, gel, overlays)
-
Practice strict hand hygiene and glove integrity checks
🧠 Bottom Line
Nail hygiene in the surgical space isn’t about appearance—it’s about protecting patients. Even one overlooked fingernail can change a life.
📚 References
-
Moolenaar, R. L., et al. (2000). A prolonged outbreak of Pseudomonas aeruginosa in a neonatal intensive care unit: did staff fingernails play a role? Infection Control and Hospital Epidemiology, 21(2), 80–85.
https://doi.org/10.1086/501745 -
Hedderwick, S. A., et al. (2000). Pathogenic organisms associated with artificial fingernails worn by healthcare workers. Infection Control and Hospital Epidemiology, 21(8), 505–509.
https://doi.org/10.1086/501795 -
Centers for Disease Control and Prevention (CDC). (2002). Guideline for Hand Hygiene in Health-Care Settings. MMWR Recommendations and Reports, 51(RR-16), 1–45.
https://www.cdc.gov/handhygiene/ -
Association of periOperative Registered Nurses (AORN). (2023). Guideline for Hand Hygiene.
https://www.aorn.org/guidelines -
Australian College of Perioperative Nurses (ACORN). (2023). Standards for Perioperative Nursing in Australia.
https://www.acorn.org.au/standards -
Alberta Health Services. (2020). Artificial Nails and Nail Polish in Healthcare Settings – Fact Sheet.
https://www.albertahealthservices.ca/assets/info/hp/hh/if-hp-hh-artificial-nails-in-healthcare.pdf -
World Health Organization (WHO). (2009). WHO Guidelines on Hand Hygiene in Health Care.
https://www.who.int/publications/i/item/9789241597906 -
Scott, R. D. (2009). The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. CDC.
https://stacks.cdc.gov/view/cdc/11550 -
Kaye, K. S., et al. (2009). The Cost of Surgical Site Infections in the United States. Infection Control and Hospital Epidemiology.
https://www.wired.com/2009/12/one-surgical-infection-with-mrsa-61000 -
Magill, S. S., et al. (2014). Multistate Point-Prevalence Survey of Health Care–Associated Infections. New England Journal of Medicine, 370, 1198–1208.
https://www.cdc.gov/hai/data/portal/index.html -
Graves, N., Halton, K., & Lairson, D. R. (2007). The economics of infection control: Hospital-acquired infections and patient safety. Current Opinion in Infectious Diseases, 20(4), 337–341.
https://doi.org/10.1097/QCO.0b013e3282638e25 -
Gillespie, B. M., et al. (2021). The Burden of Surgical Site Infections in Australia: A Cost of Illness Study. Australian and New Zealand Journal of Surgery, 91(3), 387–392.
https://doi.org/10.1111/ans.16339 -
Infection Control Today. (2001). Artificial Nails Undermine Infection Control.
https://www.infectioncontroltoday.com/view/artificial-nails-undermine-infection-control -
CIDRAP. (2023). Study: Healthcare-Linked Infections Cost US $10 Billion a Year.
https://www.cidrap.umn.edu/clostridium-difficile/study-healthcare-linked-infections-cost-us-10-billion-year