Why Caring for Surgical Instruments Matters: Safety, Efficiency & Smarter Costs
Posted at 25 July 2025 in Clinical Quality & Safety,Perioperative Practice by Marrianne
🔍 Introduction
Surgical instruments are designed to be precise and effective. Whether it’s a scalpel, forceps, or clamps, these tools must be clean, sterile, and in optimal condition to perform their functions. Any deviation from these standards can compromise a surgery’s success.
Neglecting proper maintenance can result in dull blades, rusted surfaces, or—worse—the presence of harmful microorganisms. This not only jeopardizes patient health but also tarnishes the trust patients place in healthcare providers.
Instruments that don’t cut, grip, or function as intended don’t just slow down the procedure—they create clinical risk, frustrate teams, and undermine the flow of surgery. The solution? Consistent, evidence-based maintenance practices that protect performance and patient care.
1. Patient Safety & Clinical Outcomes
-
Poor-quality or poorly maintained instruments are directly linked to adverse safety incidents.
-
Between 2004–2010, the NHS reported over 2,000 surgical incidents involving instrument failure, leading to reoperations, retained fragments, and moderate to severe harm.
-
The U.S. FDA documents hundreds of similar events annually—ranging from infection and tissue injury to fatal outcomes caused by instrument malfunction or debris.
-
Instruments that are dull or contaminated increase the risk of postoperative infections, tissue trauma, and delayed healing—all of which can compromise recovery and the patient experience.
-
Cleanliness and condition aren’t cosmetic—they are foundational to safe surgical practice.
2. Operational Efficiency & Surgical Flow
-
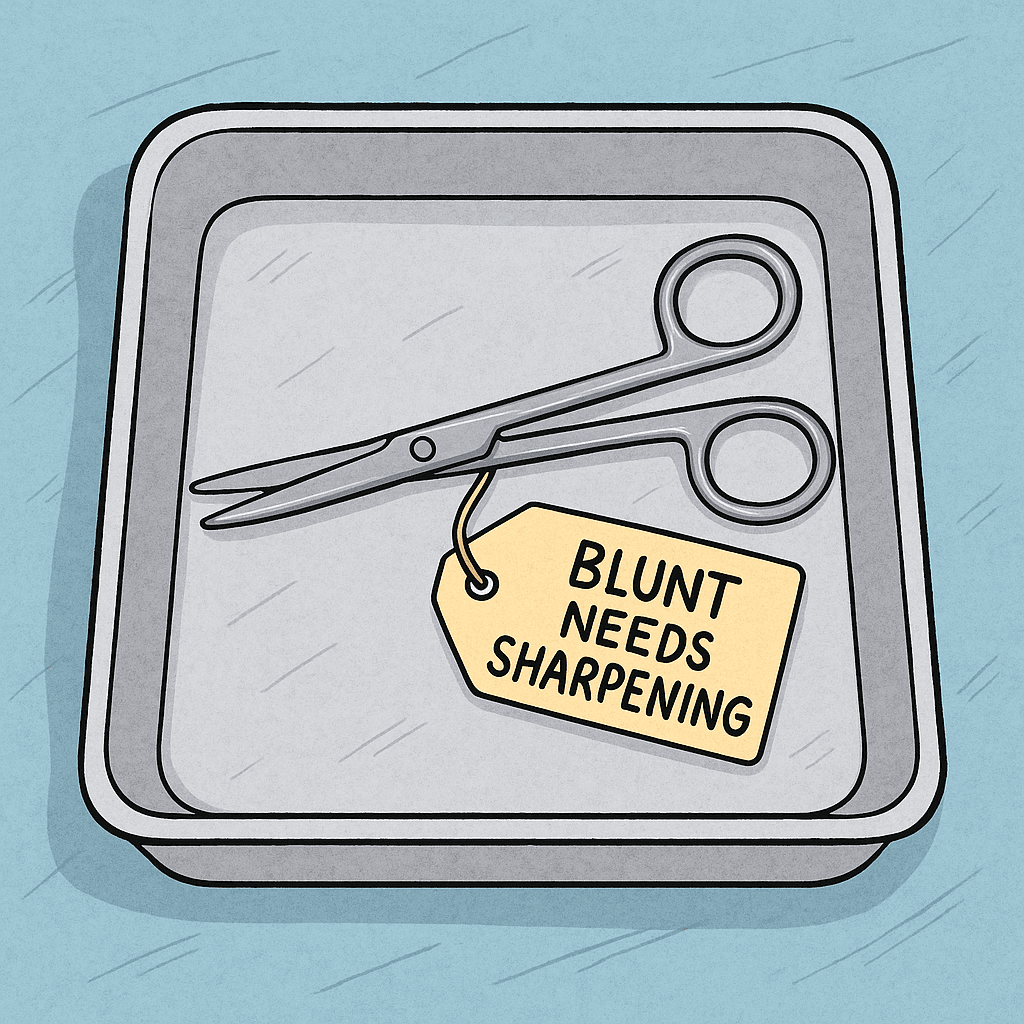
A blunt scissor or malfunctioning clamp can delay critical steps in surgery.
-
When surgical flow is interrupted, anesthesia time increases, procedural accuracy may decline, and tension among staff can escalate.
-
Tray inefficiencies (e.g., including instruments never used) add to setup, sterilization, and audit burdens.
-
Optimizing trays and removing redundant tools can reduce setup time by up to 40% and cut processing costs by 30–60%.
3. Cost Containment & Lifecycle Savings
-
Repair vs. replace: Repaired instruments can cost 30–40% less per use compared to always replacing them.
-
Facilities that implemented preventive maintenance programs reported annual savings of up to $250,000, simply by reducing waste, delay, and loss.
-
Each minute of OR time costs an average of $36–$46 USD. A malfunctioning instrument that causes a 3-minute delay could cost $100+ per case—not counting the clinical risks involved.
4. Infection Control & Regulatory Alignment
-
Instruments with dried biological material or rusted surfaces are more difficult to clean and sterilize—posing infection risks.
-
Compliance with infection control policies, such as those from AORN, ACORN, and WHO, require validated reprocessing and functional assurance for every tool.
-
Instruments must be traceable, inspected, and documented—especially following a reported breach or surgical incident.
✅ What Effective Instrument Care Looks Like
| Best Practice | Impact |
|---|---|
| Scheduled sharpening, function testing | Ensures sharpness, grip, and safe operative performance |
| Tray optimization & instrument rationalization | Reduces waste, speeds up processing, cuts costs |
| Strict cleaning & inspection protocols | Minimizes infection risk and instrument failure |
| Documentation & traceability systems | Supports quality audits and incident tracking |
| Collaboration between SPD and OR teams | Flags instruments before cases, avoids intra-op delays |
🧠 Conclusion
Caring for surgical instruments is not a backroom task—it’s a frontline safety measure.
-
🛡️ Patients deserve sterile, sharp, safe instruments.
-
🔄 Teams deserve tools they can trust.
-
💰 Facilities benefit from cost control, efficiency, and reduced risk.
Investing in instrument care is a small effort with a massive return—one that protects patients, supports surgical teams, and sustains clinical excellence.
🔗 References
-
Association of periOperative Registered Nurses (AORN). (2022). Guidelines for Perioperative Practice. AORN, Inc.
-
Australian College of Perioperative Nurses (ACORN). (2023). Standards for Perioperative Nursing in Australia.
-
Microlin Surgical. (2021). Instrument Maintenance Cost and Lifecycle Analysis. Retrieved from https://www.microlinesurgical.com
-
Bausch & Lomb Instruments. (2020). Managing Surgical Instruments for Optimal Performance. Retrieved from https://www.bauschinstruments.com
-
Applied Physics Medical. (2021). How Surgical Instruments Impact Patient Outcomes. Retrieved from https://appliedphysicsmedical.com
-
Rick Schultz. (2019). The Instrument Whisperer: Why Instrument Quality Matters. Healthcare Purchasing News.
-
Sullivan Healthcare Consulting. (2020). How a Large Academic Medical Center Uncovered $250,000 in Annual Cost Savings. Retrieved from https://sullivanhealthcareconsulting.com
-
Journal of Arthroplasty. (2021). Cost Analysis of Operating Room Time and Efficiency. https://www.arthroplastyjournal.org
-
Duke University Medical Center. (2022). Analysis of Surgical Instrument-Related Adverse Events in U.S. Hospitals. Retrieved from https://dukespace.lib.duke.edu
-
Infection Control Today. (2022). Best Practices in Surgical Instrument Reprocessing. https://www.infectioncontroltoday.com
-
World Health Organization (WHO). (2009). Surgical Safety Checklist and Infection Control Guidelines. https://www.who.int
-
OR Today Magazine. (2019). The Real Cost of an OR Minute. Retrieved from https://ortoday.com
Recent Articles
Electrosurgery & Cautery Safety: Protecting Patients Through Vigilance, Communication, and Best Practice
09 December 2025
✈️From Pilots to Perioperative Practice: Why Organisation and Readiness Save Lives in the OR
28 October 2025
Categories
More articles from Clinical Quality & Safety,Perioperative Practice
View AllElectrosurgery & Cautery Safety: Protecting Patients Through Vigilance, Communication, and Best Practice
⭐ A Personal Note on Perioperative Practice Every day in the operating room, perioperative professionals carry a...
09 December 2025
Read more✈️From Pilots to Perioperative Practice: Why Organisation and Readiness Save Lives in the OR
Instrument nurses anticipate, troubleshoot, and act quickly under the direction of the surgeon and surgical team. T...
28 October 2025
Read more🚫 Artificial Nails in the Operating Room: More Than a Policy—It’s a Patient Safety Imperative
In perioperative environments, details matter—especially those that impact infection prevention and patient safet...
30 July 2025
Read more