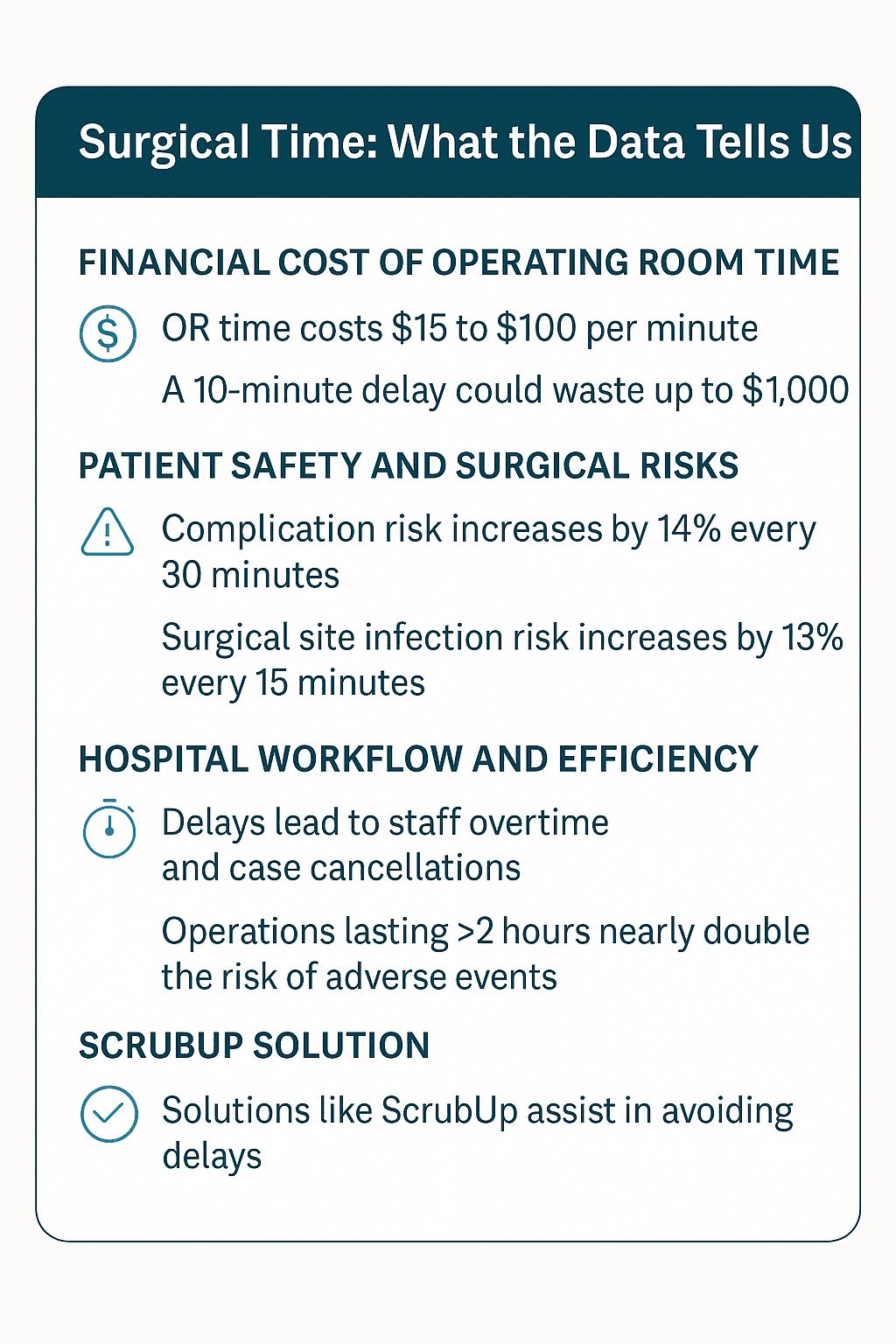
⏱️ Every Minute Matters: The True Cost of Surgical Time
In the operating room, time is more than just a metric — it’s a matter of cost, safety, and care. Every additional minute a patient spends under anesthesia increases the financial burden on healthcare systems and escalates the risk of complications. Whether it’s a delay due to missing instruments or a scheduling backlog, the consequences of lost OR time are profound.
💰 The Financial Toll of Operating Room Time
Research estimates that each minute of operating room time costs between $15 and $100. A U.S. hospital survey reported an average OR charge of $62 per minute, with high-complexity surgeries topping $133/minute. That means a 10-minute delay could cost up to $1,000 — money lost on idle staff, extended prep, or inefficient scheduling.
Hospitals absorb these costs in the form of overtime wages, surgical backlogs, and reduced daily throughput. One U.S. health system lost 631 hours of OR time and nearly $390,000 annually due to late starts for the first case of the day.
⚠️ Time and Patient Safety Are Inseparable
The longer a patient is on the operating table, the higher their risk of harm. Compelling data supports this:
-
Surgical complication risk increases by 14% for every 30 extra minutes in the OR.
-
Surgical site infections rise by 13% for every additional 15 minutes.
-
When surgeries exceed 2 hours, the risk of adverse events nearly doubles.
Extended surgical duration not only affects clinical outcomes but also contributes to longer recovery stays, increased bed blockages, and greater pressure on postoperative teams.
🚨 The Ripple Effect of Delay
Delays in the OR don’t just affect one case — they cascade across the entire surgical schedule. Late starts, case overruns, and equipment errors result in:
-
Cancelled surgeries, extending waitlists and frustrating patients.
-
Overtime labor, straining budgets and causing staff burnout.
-
Reduced surgical throughput, which means fewer patients treated each day.
Hospitals aiming to optimize their workflow must treat OR time as the limited, high-value resource it is.
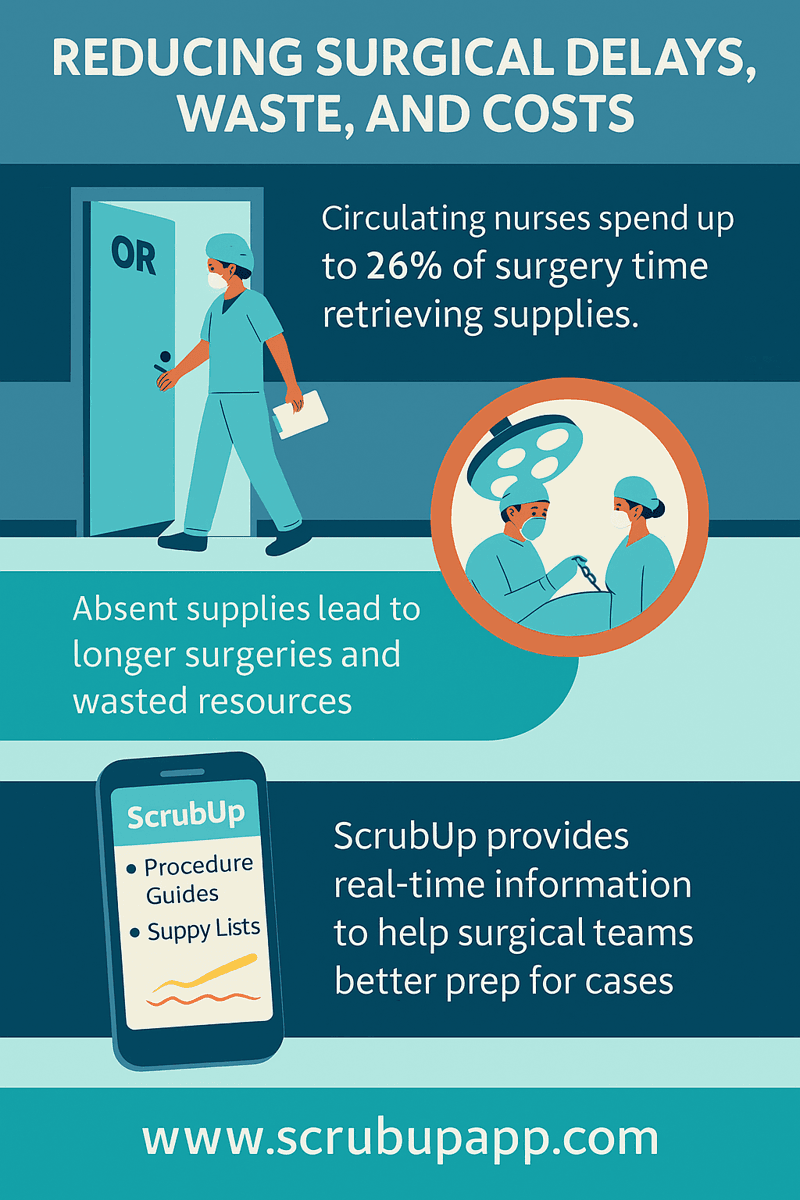
✅ ScrubUp: Optimizing Every Surgical Minute
This is where ScrubUp steps in. ScrubUp is a digital platform built to support surgical teams with real-time preparation, streamlined equipment checklists, and surgeon preference tracking. By ensuring all surgical setup details are documented, shared, and ready ahead of time, ScrubUp eliminates the most common delays.
Because in the OR, the loss of one minute can mean the loss of a life or a limb.