🌟 Building Competence in the OR Takes Time—And Pays Off
Posted at 27 October 2025 in Perioperative Education,Professional Development by Marrianne
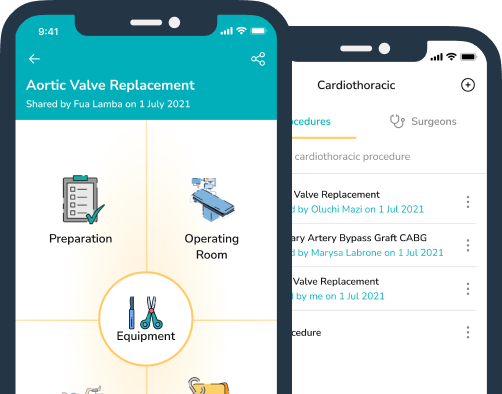
Instrument and circulator nurses and technologists perform some of the most complex, high-pressure roles in healthcare. Their work demands clinical competence, situational awareness, and theory-based practice—skills that take time, mentorship, and structured exposure across multiple surgical specialties to develop.
For example:
-
🩺 Perioperative nurses: structured programs (AORN Periop 101, ACORN transition programs, UK AfPP Frameworks, EORNA and ORNAC competency guidelines) typically span 6–12 months of intensive training, with an additional 12–24 months to build independent multi-specialty proficiency.
-
🧰 Surgical technologists/instrument nurses: require 12–24 months of formal education plus continuing clinical mentorship to achieve advanced practice levels.
Healthcare facilities that invest beyond orientation—offering rotational learning, mentorship, and team-training—see measurable benefits:
✅ Stronger safety culture and teamwork
✅ Reduced surgical complications and near-misses
✅ Improved staff confidence, engagement, and retention
When organisations fail to train and rotate junior or novice staff appropriately, senior “all-rounders” end up carrying the load. This imbalance leads to burnout, turnover, and risk to patient safety.
By contrast, structured perioperative education—aligned with AORN, ACORN, AfPP, EORNA, and ORNAC standards—builds teams that are competent, confident, and collaborative, ultimately delivering higher standards of surgical care.
Investing in time-based competence is not a cost—it’s patient safety assurance.
📚 Selected References
-
AORN (US): Perioperative 101 Program & RN Residency Guidelines (6–12 months structured training).
-
ACORN (Australia): Standards for Perioperative Nursing Practice (2024)—competency-based education and role delineation.
-
AfPP (UK): Perioperative Career Framework (2022)—progressive skill development across roles.
-
EORNA (Europe): Core Curriculum for Perioperative Nursing (2019)—emphasises mentorship and safety culture.
-
ORNAC (Canada): Standards, Guidelines and Position Statements (2021)—education and safe practice framework.
-
Team-training outcomes: WHO Surgical Safety Checklist (NEJM 2009); VA Medical Team Training Program (JAMA 2010)—linked to lower surgical mortality and improved teamwork.
🩺 #PerioperativeNursing #OperatingRoom #SurgicalTeamwork #ClinicalEducation #PatientSafety #NurseLeadership #ScrubNurse #CirculatorNurse #SurgicalTechnologist #HealthcareCulture #BurnoutPrevention
Recent Articles
Electrosurgery & Cautery Safety: Protecting Patients Through Vigilance, Communication, and Best Practice
09 December 2025
✈️From Pilots to Perioperative Practice: Why Organisation and Readiness Save Lives in the OR
28 October 2025
Why Interruptions in the Operating Room Put Safety, Efficiency, and Staff Wellbeing at Risk
26 September 2025
Categories
More articles from Perioperative Education,Professional Development
View All📚 Why Time and Education Matter in Instilling Best Practice
Embedding best practices into clinical skills requires deliberate time investment, structured education, and ongoin...
30 June 2025
Read moreReducing SSIs Through Best Practice Skin Preparation: What Every OR Nurse Should Know
Best Practice for Surgical Skin Preparation: Reducing the Risk of Surgical Site Infections (SSIs) Surgical skin pr...
11 June 2025
Read more