Communication in the OR
Posted at 21 May 2024 in Operating Room,Patient Safety by Marrianne
 The operating room is a culturally diverse background with various levels of multidisciplinary professionals working collaboratively to deliver optimized care.
The operating room is a culturally diverse background with various levels of multidisciplinary professionals working collaboratively to deliver optimized care.
A study by the British Journal of Anaesthesia, identifies;
- Failures in peri-operative communication contributed to patient injury in 43% of 910 anaesthesia malpractice claims
- The most common root cause of communication failure was insufficient or inaccurate information, occurring in 30% of procedures
As part of a team that assessed RCA’s and near misses, communication was highlighted as a contributing factor in a majority of cases. Nurses stated they did not feel heard and confident, especially as a novice.
Surgeons may also feel unsupported by staff they are unfamiliar with or who are unfamiliar with the flow of surgery.
We need to empower all operating room professionals to work collaboratively, but we also need to empower and provide knowledge and support to our clinicians, in order to support, and deliver enhanced patient care.
The annual cost of medical errors likely exceeds $17 billion, with 35% being surgery related
A recent publication, Towards the Future of Surgery, 2024 has highlighted the need for surgeons to further develop their soft skills.
This is something we should all consider. Here’s a little insight.
“It is clear how patient outcomes are becoming less and less dependent on technical skills (however, this is always essential) and increasingly dependent on non-technical skills. Surgeons have the potential to improve patient outcomes, reduce medical errors, and improve patient satisfaction through their leadership on the multidisciplinary team.”
“Leadership in surgery entails many non-technical skills, including professionalism, technical competence, motivation, innovation, teamwork, communication skills, decision making, business acumen, ethics, emotional competence, resilience and effective teaching.”
“Surgeons have the potential to improve patient outcomes, reduce medical errors, and improve patient satisfaction through their leadership on the multidisciplinary team.”
I believe we all have the ability to improve patient outcomes.
Our use of checklists, such as the Surgical Safety Checklist has reduced errors by 30%.
Research shows we can improve patient outcomes by developing a team culture by easily identifying surgical team members, via scrub or cap identification.
Team huddle has also improved team collaboration and work flow.
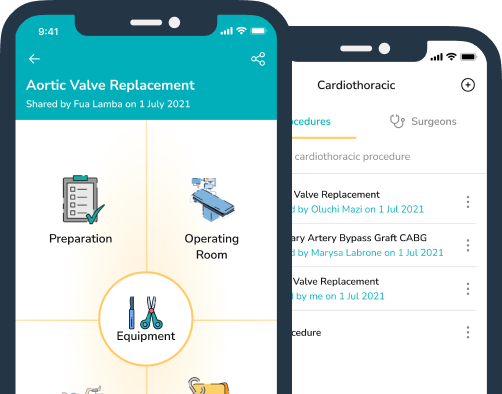
Effective communication aims to streamline practices and utilizing resources to share information is key when stakes and patient lives are at risk.
Lets all aim to improve communication, empower clinicians and share our clinical expertise.
ttps://www.bjanaesthesia.org.uk/article/S0007-0912(21)00349-4/fulltext
Towards the Future of Surgery, 2024
Recent Articles
Electrosurgery & Cautery Safety: Protecting Patients Through Vigilance, Communication, and Best Practice
09 December 2025
✈️From Pilots to Perioperative Practice: Why Organisation and Readiness Save Lives in the OR
28 October 2025
Categories
More articles from Operating Room,Patient Safety
View All✈️From Pilots to Perioperative Practice: Why Organisation and Readiness Save Lives in the OR
Instrument nurses anticipate, troubleshoot, and act quickly under the direction of the surgeon and surgical team. T...
28 October 2025
Read moreWhy Interruptions in the Operating Room Put Safety, Efficiency, and Staff Wellbeing at Risk
The Hidden Cost of Interruptions in the OR: Why Focus Matters Imagine this: mid-operation, a circulator is execu...
26 September 2025
Read moreSurgical Site Infections: Reducing the Burden Through Teamwork and Collaboration
Introduction Surgical Site Infections (SSIs) are among the most common healthcare-associated infections worldwide....
28 August 2025
Read more The operating room is a culturally diverse background with various levels of multidisciplinary professionals working collaboratively to deliver optimized care.
The operating room is a culturally diverse background with various levels of multidisciplinary professionals working collaboratively to deliver optimized care.