Embedding best practices into clinical skills requires deliberate time investment, structured education, and ongoing reinforcement. Research indicates that:
-
🔍 Deliberate practice over time improves clinical performance.
Ericsson et al.’s seminal work on skill acquisition demonstrates that expert performance arises from structured, repetitive practice—not merely experience. In surgical settings, this entails building skills through repeated exposure to procedural norms, instrument setup, and workflow protocols.
(Ericsson KA et al., 1993. Psychological Review) -
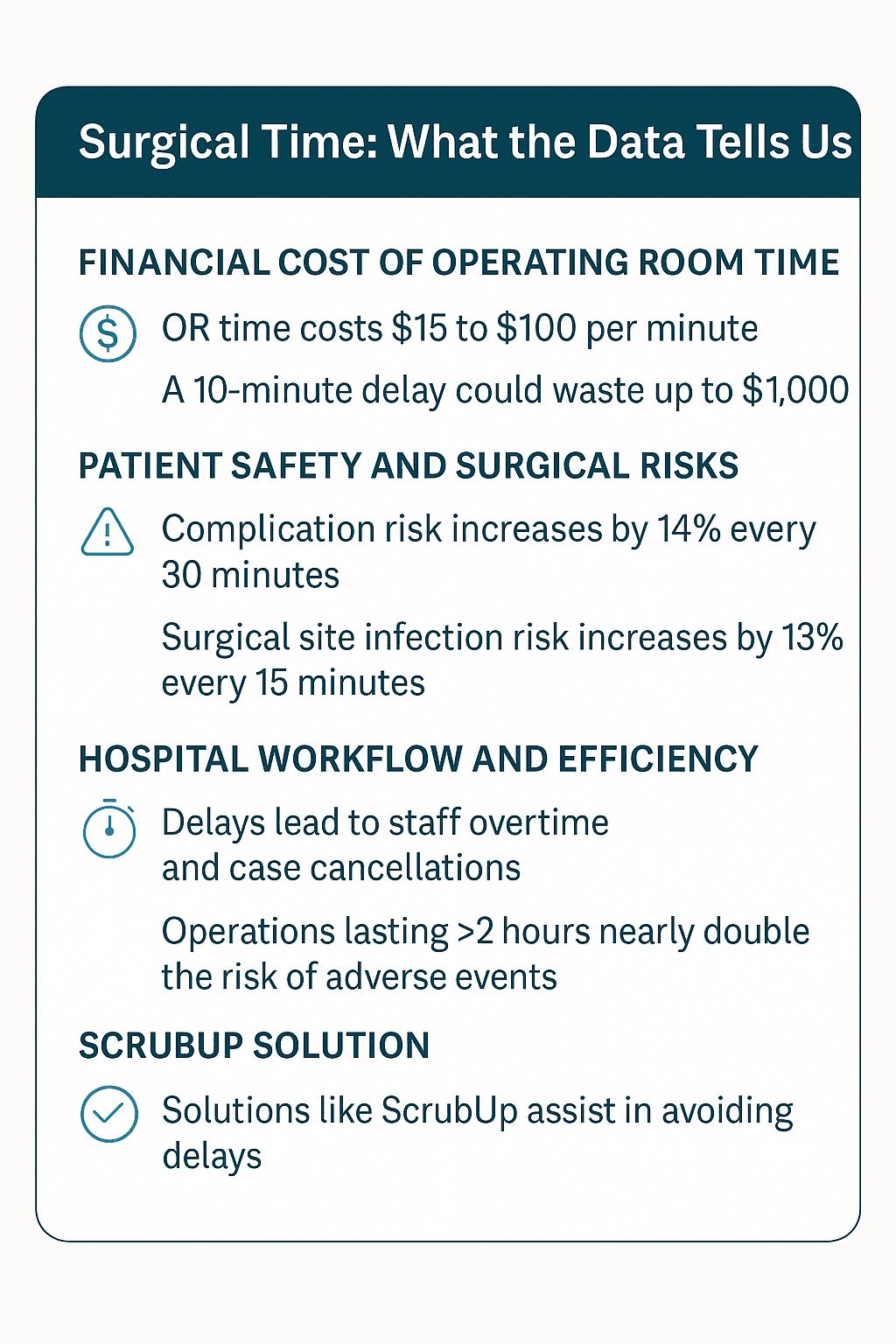
🕒 Operating rooms are complex environments with high cognitive demands.
A prospective observational study by Göras et al. (2019) found that surgical teams performed an average of 64 tasks per hour, with nearly half involving communication. Multitasking accounted for 48.2% of the time, and interruptions occurred at a rate of 3.0 per hour, predominantly due to equipment issues. These findings highlight the necessity for structured education and time allocation to manage the complexities of the OR effectively.
(Göras C et al., 2019. BMJ Open) -
🧠 Simulation and structured education improve retention of best practices.
A study in the Journal of the American College of Surgeons found that OR team members who engaged in simulation-based education were more likely to adhere to best practice protocols, such as surgical safety checklists and aseptic setup techniques.
(Barsuk JH et al., 2009. J Am Coll Surg) -
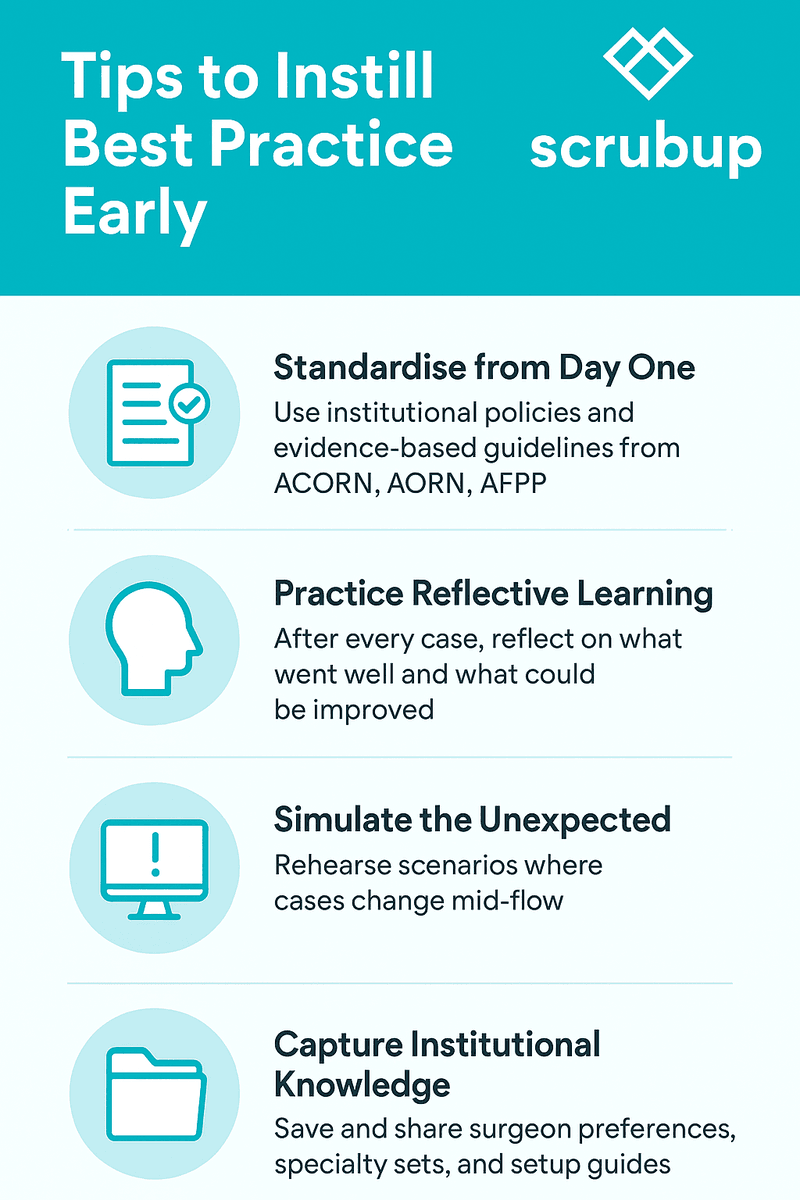
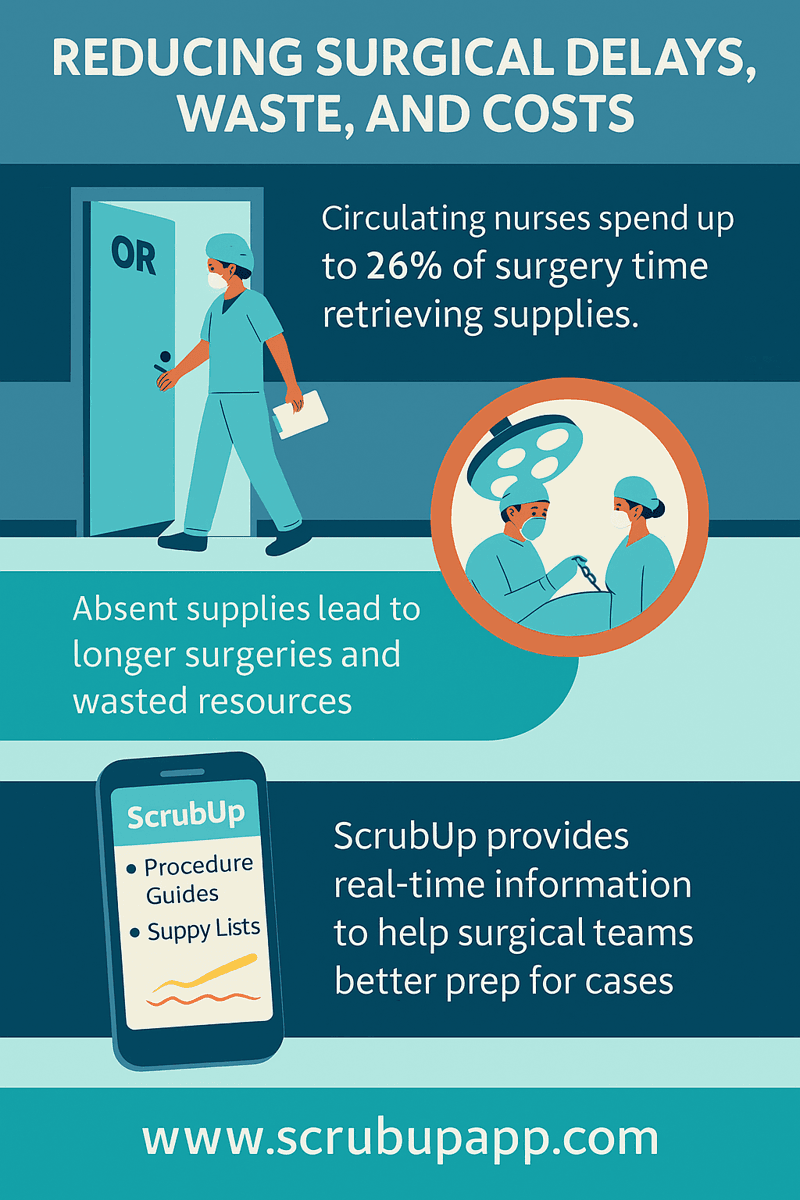
📈 Structured learning platforms help consolidate complex clinical knowledge.
Digital tools that reinforce policy-based workflows (like ACORN, AORN, AFPP) assist learners in absorbing, applying, and reflecting on clinical procedures in real-time. Platforms like ScrubUp bridge the gap between formal education and day-to-day clinical needs.
Final Thought (Updated):
By investing time in education and reinforcing evidence-based standards, we don’t just teach a skill—we nurture clinical judgment, adaptability, and professionalism. Whether it’s the first surgical tray setup or a case pivot under pressure, clinicians trained with time and structure are best equipped to deliver safe, efficient care.
References:
https://psycnet.apa.org/record/1993-40718-001
https://pubmed.ncbi.nlm.nih.gov/31097486/
https://pubmed.ncbi.nlm.nih.gov/19667306/