In the high-stakes environment of the operating room (OR), every second counts. While surgeons often take center stage, it’s the cohesive effort of the entire surgical team that ensures patient safety and procedural success. Yet, this intricate dance is frequently disrupted by unforeseen challenges, leading to increased stress, potential errors, and compromised patient outcomes.
⏱️ The Hidden Costs of Operating Room Disruptions
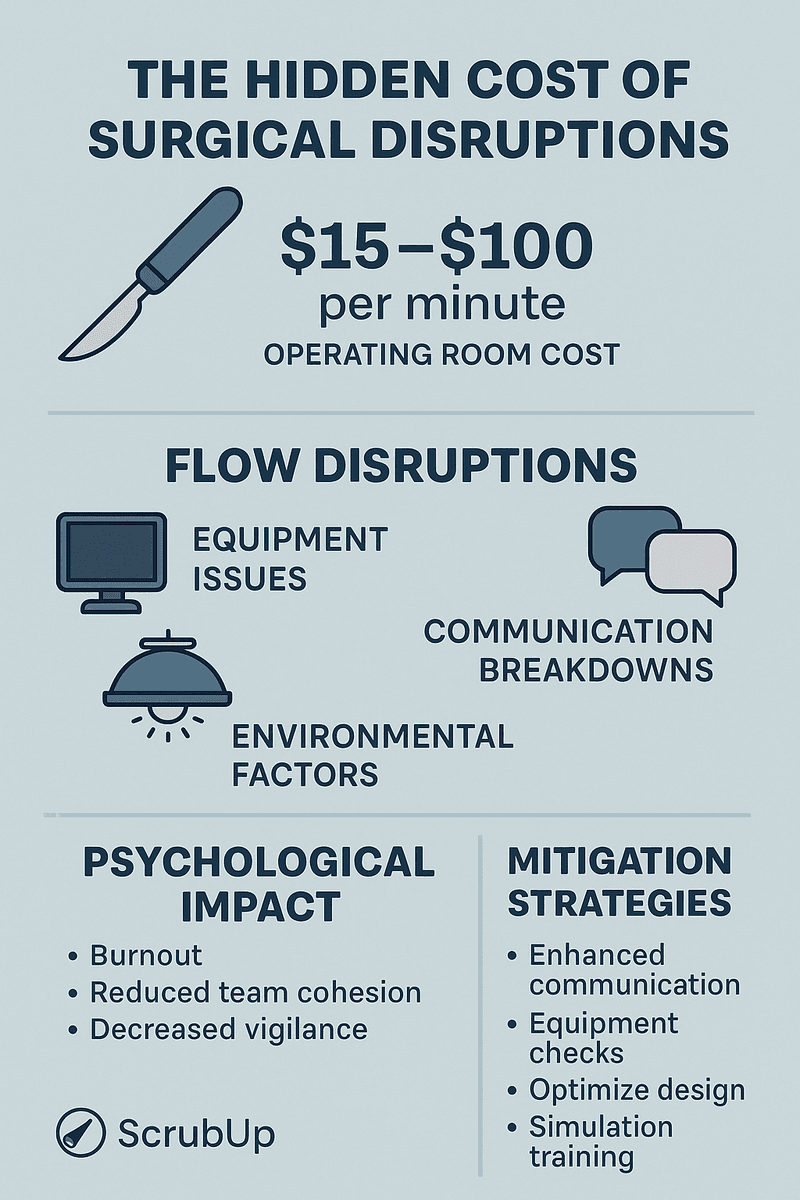
Time is a critical resource in the OR. Delays not only escalate operational costs but also heighten risks for patients. Research indicates that each minute in the OR can cost between $15 and $100, depending on the procedure and facility . Factors contributing to these costs include:
-
Extended anesthesia time: Prolonged exposure increases the risk of complications.
-
Staff overtime: Delays can lead to extended shifts, impacting staff well-being and hospital budgets.
-
Reduced surgical throughput: Fewer procedures can be completed, affecting hospital revenue and patient access to care.
🔄 Understanding Flow Disruptions
Flow disruptions (FDs) are interruptions that divert the surgical team’s attention from the primary task. These can range from equipment malfunctions to unexpected staff changes. A systematic review highlighted that FDs are associated with increased surgical duration and heightened stress levels among OR staff .
Common sources of FDs include:
-
Equipment issues: Malfunctioning or missing tools can halt procedures.
-
Communication breakdowns: Misunderstandings or lack of information sharing can lead to errors.
-
Environmental factors: Poor OR layout or lighting can impede workflow.
🧠 The Psychological Toll on Surgical Teams
Beyond the tangible delays, FDs exert a significant psychological impact on OR personnel. A study focusing on robotic-assisted surgeries found that equipment-related FDs were linked to increased staff workload . Persistent disruptions can lead to:
-
Burnout: Continuous stress without adequate recovery can diminish job satisfaction.
-
Reduced team cohesion: Frequent interruptions can strain professional relationships.
-
Decreased vigilance: Over time, constant disruptions may desensitize staff to potential hazards.
🛠️ Strategies for Mitigating Disruptions
Addressing FDs requires a multifaceted approach:
-
Enhanced Communication Protocols: Implementing standardized communication tools, like checklists, can ensure all team members are aligned.
-
Regular Equipment Maintenance: Routine checks can preempt equipment failures.
-
OR Design Optimization: Adjusting the physical layout can streamline workflows and reduce unnecessary movements.
-
Training and Simulation: Regular drills can prepare teams to handle unexpected disruptions effectively.
📈 The Role of Technology in Streamlining OR Processes
Digital solutions, such as ScrubUp, offer platforms to:
-
Track surgical instruments: Ensuring all necessary tools are available and functional.
-
Manage team schedules: Coordinating staff shifts to maintain consistency.
-
Provide real-time updates: Keeping all team members informed about procedural changes or patient status.
By integrating such technologies, hospitals can reduce the frequency and impact of FDs, leading to improved patient outcomes and enhanced team morale.
🩺 Conclusion
The efficiency of the OR hinges not just on the surgeon’s skill but on the seamless collaboration of the entire surgical team. Recognizing and addressing the challenges posed by flow disruptions is paramount. Through proactive measures, continuous training, and the adoption of innovative technologies, we can foster an environment where both patients and healthcare professionals thrive.
https://qualitysafety.bmj.com/content/29/12/1033
https://link.springer.com/article/10.1007/s00464-023-10162-2